Does calf pain always mean a DVT?
No, calf pain does not always mean you have a deep vein thrombosis (DVT). While the calf is the most common location for a blood clot, pain in this area is frequently caused by less serious issues such as muscle strains, ‘charley horse’ cramps, or minor injuries. However, because a DVT can be life-threatening if it travels to the lungs, it is essential to understand the specific characteristics that distinguish a clot from a simple muscle ache.
What We’ll Discuss in This Article
- Common non-clot causes of calf pain
- Distinguishing features of DVT versus muscle strain
- The role of unilateral swelling in identifying blood clots
- Why ‘cramp-like’ pain that persists is a clinical warning sign
- Physical triggers and risk factors that increase DVT likelihood
- Identifying inflammation and other vascular issues in the calf
- When calf pain requires an emergency medical assessment
Differentiating Between DVT and Muscle Pain
Calf pain indicates a DVT only in a minority of cases, but it requires careful evaluation if the pain is accompanied by swelling, redness, or warmth in only one leg. Unlike a muscle strain, which usually follows a specific movement or injury, DVT pain often develops without an obvious cause and persists even when the leg is at rest.
When you pull a muscle, the pain is usually sharp and occurs at a specific moment of exertion. In contrast, a blood clot creates a dull, heavy ache or a feeling of intense tightness that may worsen when you flex your toes upward. If the pain is localized to the calf but the entire lower leg feels tight or looks larger than the other side, the clinical suspicion for a DVT increases significantly.
Common Causes of Non-Clot Calf Pain
Most calf pain is musculoskeletal or related to minor circulatory issues rather than a dangerous blockage. Identifying these common triggers can help provide clarity when a sudden ache occurs.
- Muscle Strain: Tearing of the gastrocnemius or soleus muscles, often during sports or sudden movements.
- Cramps: Involuntary muscle contractions caused by dehydration, electrolyte imbalances, or fatigue.
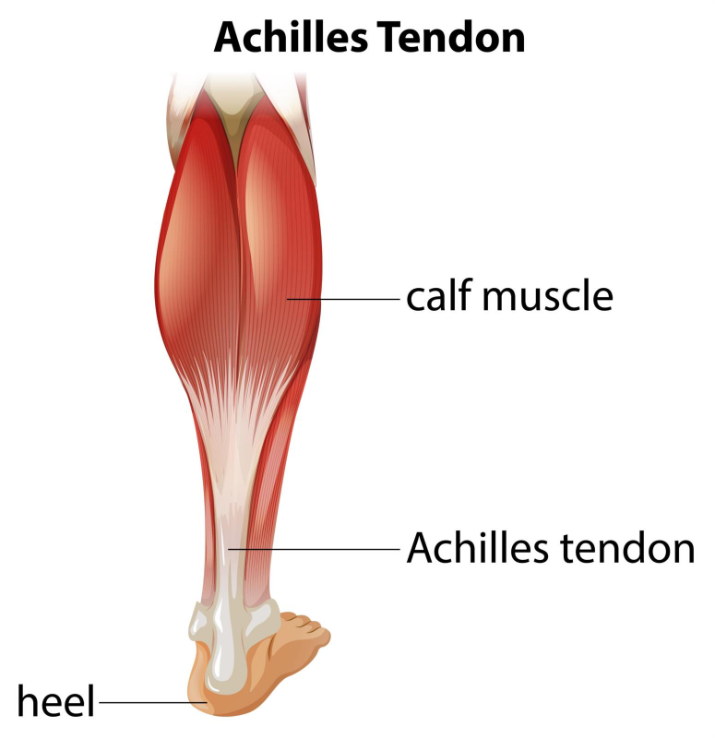
- Achilles Tendonitis: Inflammation of the tendon at the back of the ankle that can radiate pain into the lower calf.
- Baker’s Cyst: A fluid-filled sac behind the knee that, if it ruptures, can cause sudden calf pain and swelling.
- Peripheral Arterial Disease (PAD): Narrowing of the arteries that causes cramping during walking, which subsides with rest.
Triggers and Risk Factors for DVT
While calf pain can happen to anyone, certain triggers significantly increase the statistical likelihood that the pain is caused by a deep vein clot. A DVT rarely occurs in a completely healthy, active person without an underlying risk factor or a recent event that slowed blood flow.
| Risk Factor | Why it Triggers DVT |
| Recent Surgery | General anaesthesia and immobility slow down the blood. |
| Long-Distance Travel | Sitting for over four hours prevents the ‘calf pump’ from working. |
| Pregnancy | Hormonal changes and pressure on pelvic veins slow blood return. |
| Hospitalisation | Extended periods of bed rest are a primary trigger for clots. |
| Active Cancer | Certain treatments and the disease itself make blood ‘stickier’. |
If your calf pain starts after one of these events particularly a long flight or a recent operation the pain should be treated with much higher clinical urgency than a standard muscle ache.
Differentiation: DVT vs. Superficial Phlebitis
It is also important to distinguish between a clot in the deep veins (DVT) and a clot in the veins near the surface, known as superficial thrombophlebitis. While both can cause pain in the calf area, their risks and presentations differ.
Superficial phlebitis usually feels like a hard, painful ‘string’ or cord just under the skin. The skin over the vein is often very red and hot. While painful, these are generally less dangerous than a DVT. A DVT, however, involves the larger veins deep inside the muscle; the pain is often deeper, and the swelling involves the whole limb rather than just a localized red line.
My final conclusion
Calf pain is a common symptom with many causes, most of which are musculoskeletal and not life-threatening. However, the presence of unilateral swelling, skin warmth, and persistent aching especially following a period of immobility are clinical indicators that the pain may be a DVT. Distinguishing between a simple cramp and a vascular emergency is vital for ensuring timely treatment and preventing complications like pulmonary embolism.
If you experience severe, sudden, or worsening symptoms, call 999 immediately. This is especially urgent if calf pain is accompanied by sudden shortness of breath or chest pain.
Can I walk off a DVT?
No, walking will not resolve a clot; in fact, if a DVT is present, excessive exertion could potentially cause a piece of the clot to break off.
Does DVT pain always feel like a cramp?
Many patients describe it as a ‘charley horse’ that won’t go away, but it can also feel like a heavy, throbbing pressure.
Doctor Stefan, is it a DVT if both calves ache?
It is very rare for a DVT to occur in both legs at once; bilateral pain is more commonly linked to exercise, dehydration, or systemic issues.
Can a DVT be painless?
Yes, approximately half of all people with a DVT experience few or no noticeable symptoms until a complication occurs.
Why does my calf feel hot if it’s a clot?
The body creates an inflammatory response to the blockage, which increases blood flow to the surface tissues, making them feel warm.
Authority Snapshot
This article is reviewed by Dr. Rebecca Fernandez to ensure accurate clinical differentiation between musculoskeletal calf pain and deep vein thrombosis. The content focuses on evidence-based ‘red flag’ symptoms and risk factors to help the public understand when calf pain requires urgent medical attention. Dr. Rebecca Fernandez is a UK-trained physician with an MBBS and experience in general surgery, cardiology, internal medicine, gynecology, intensive care, and emergency medicine. She has managed critically ill patients, stabilised acute trauma cases, and provided comprehensive inpatient and outpatient care. In psychiatry, Dr. Fernandez has worked with psychotic, mood, anxiety, and substance use disorders, applying evidence-based approaches such as CBT, ACT, and mindfulness-based therapies. Her skills span patient assessment, treatment planning, and the integration of digital health solutions to support mental well-being.

