What increases the risk of developing DVT in the UK?
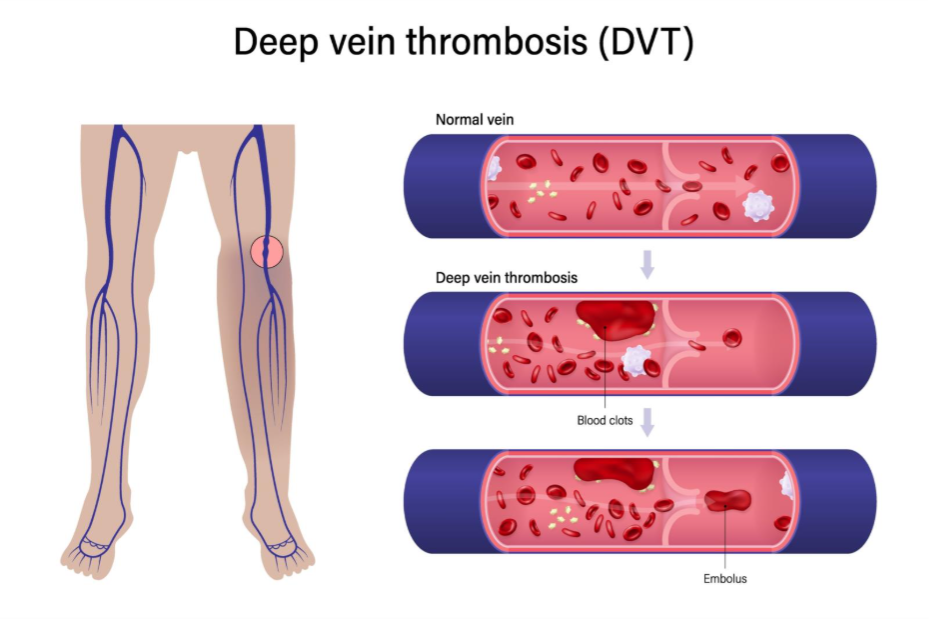
Deep Vein Thrombosis (DVT) occurs when a blood clot forms in a deep vein, typically in the leg. In the UK, this condition remains a significant public health concern, often serving as the precursor to a pulmonary embolism. Understanding what increases your risk is essential for prevention, especially for those with sedentary lifestyles or upcoming surgical procedures. This article explores the biological, environmental, and medical factors that contribute to clot formation.
What We’ll Discuss in This Article
- The primary medical and lifestyle risk factors for DVT.
- How immobility and travel impact blood flow in the deep veins.
- The role of hormones and pregnancy in increasing blood viscosity.
- Genetic predispositions common in the UK population.
- How to differentiate DVT symptoms from common muscle strains.
- Preventative measures to mitigate risk during high-risk periods.
Primary Risk Factors for DVT
You are at an increased risk of developing DVT if you are over 60, smoke, are overweight, or have a family history of blood clots. Medical conditions such as heart failure, vasculitis, and active cancer also significantly elevate risk because they change the way blood flows or how easily it clots. Furthermore, using hormonal contraceptives or hormone replacement therapy (HRT) can alter blood chemistry, making it ‘stickier’ and more prone to forming obstructions in the venous system.
In the clinical landscape of the UK, obesity is one of the most prevalent modifiable risk factors. Excess weight increases the pressure in the veins of your pelvis and legs. When combined with a sedentary desk-based work culture, the physical movement required to pump blood back to the heart is diminished. This stasis allows blood to pool, which is the first step in the formation of a thrombus.
Causes of DVT
The physiological cause of DVT is rooted in ‘Virchow’s Triad’, a trio of factors: stasis of blood flow, vessel wall injury, and hypercoagulability. Anything that slows blood flow, damages the lining of a vein, or makes the blood more likely to clot will cause a DVT.
Common causes include:
- Surgery and Trauma: Major surgery, particularly on the hips or knees, can damage veins and release clotting factors into the blood.
- Chronic Illness: Conditions like inflammatory bowel disease (IBD) or lupus create a pro-inflammatory state that encourages clotting.
- Venous Insufficiency: If the valves in your veins are weak, blood struggles to move upward, leading to pooling.
Triggers for a Blood Clot
Specific events or environmental changes often act as triggers for those already at risk. In the UK, seasonal changes and travel patterns play a role.
- Prolonged Immobility: This includes being bedbound in a hospital or sitting for long periods in a car or plane. When the calf muscles do not contract, the ‘muscle pump’ fails.
- Dehydration: This increases blood viscosity. On long journeys, the combination of cramped seating and low fluid intake is a significant trigger.
- Acute Infection: Severe infections, including recent bouts of respiratory viruses, can trigger a systemic inflammatory response that increases clotting risk for several weeks.
Differentiation: DVT vs. Muscle Strain
It is common for patients to mistake a DVT for a simple cramp or a pulled calf muscle. However, the clinical presentation differs in several key ways.
| Feature | Deep Vein Thrombosis (DVT) | Muscle Strain |
| Pain Location | Deep in the calf or thigh | Specifically where the muscle was overstretched |
| Skin Temperature | The affected area often feels warm to the touch | Usually normal temperature |
| Swelling | Often significant swelling of the entire lower leg | Localised swelling at the site of injury |
| Skin Colour | May appear red or slightly blue/purple | May show bruising, but not widespread redness |
| Pain Trigger | Pain often worsens when pulling toes upward | Pain occurs when using the specific muscle |
Conclusion
Increasing your awareness of DVT risk factors is the first step in prevention. Factors such as age, weight, and mobility are critical, but temporary triggers like surgery or long-haul travel also require vigilance. By staying hydrated and maintaining regular movement, you can significantly reduce the likelihood of a clot forming.
If you experience severe, sudden, or worsening symptoms, call 999 immediately.
Is DVT more common in men or women?
The risk is relatively equal, though women face unique risks during pregnancy or while using hormonal medications like the combined pill.
Can you have a DVT with no symptoms?
Yes, approximately half of people with DVT have no noticeable symptoms until the clot moves or causes significant swelling.
How does smoking affect DVT risk?
Smoking damages the lining of the blood vessels and affects blood clotting, making it one of the most significant avoidable risks.
Can I get DVT from a short flight?
While the risk is highest on flights over four hours, any period of total immobility can contribute to stasis in the veins.
Does caffeine increase clot risk?
Caffeine itself is not a direct cause, but its dehydrating effects can increase blood viscosity if not balanced with water. Is DVT hereditary?
Is DVT hereditary?
Yes, certain genetic conditions like Factor V Leiden, which are prevalent in some UK populations, significantly increase the blood’s tendency to clot.
Authority Snapshot
This article has been produced to provide the UK public with evidence-based information regarding venous health. It focuses on the intersection of lifestyle and clinical risk factors to help readers identify when they may be at an elevated risk. All information aligns with standard UK medical protocols for the identification of venous thromboembolism. Dr. Rebecca Fernandez is a UK-trained physician with an MBBS and experience in general surgery, cardiology, internal medicine, gynecology, intensive care, and emergency medicine. She has managed critically ill patients, stabilised acute trauma cases, and provided comprehensive inpatient and outpatient care. In psychiatry, Dr. Fernandez has worked with psychotic, mood, anxiety, and substance use disorders, applying evidence-based approaches such as CBT, ACT, and mindfulness-based therapies. Her skills span patient assessment, treatment planning, and the integration of digital health solutions to support mental well-being.

