Can fainting or slow heartbeat mean a pacemaker is needed?
Fainting and a slow heartbeat are two of the most common clinical indicators that a person may require a pacemaker. In the UK, a slow heart rate, known as bradycardia, is often the result of the heart’s natural electrical system failing to send signals effectively. When the heart cannot maintain a sufficient rate to pump oxygenated blood to the brain, it can lead to temporary loss of consciousness, known as syncope or fainting.
In this article, you will learn why these symptoms occur, the specific heart rhythm conditions they point to, and the criteria UK clinicians use to recommend a pacemaker. We will also explore the underlying causes of electrical failure in the heart, common triggers for fainting episodes, and how a pacemaker differs from other treatments.
What We’ll Discuss in This Article
- The relationship between bradycardia and fainting episodes
- Clinical conditions such as heart block and sick sinus syndrome
- Why a slow heart rate leads to dizziness and lack of energy
- Common causes of electrical conduction failure in the heart
- Environmental and physical triggers for symptomatic slow heartbeats
- How a pacemaker restores a normal heart rhythm
- Emergency guidance for sudden blackouts or severe symptoms
Why a slow heartbeat leads to fainting
A slow heartbeat, typically defined as fewer than 60 beats per minute at rest, can be normal for athletes but may be problematic for others. If the heart rate drops too low, the brain does not receive enough oxygen, which is the direct cause of fainting. This is the body’s emergency response to ensure blood flow reaches the brain by bringing the person to a horizontal position.
If you experience fainting (syncope) alongside a documented slow heartbeat, it often suggests that the heart’s ‘internal wiring’ is failing. This might manifest as long pauses between beats or a rate that fails to increase during physical activity. In the UK, if these symptoms are frequent or put the patient at risk of injury, a pacemaker is usually the recommended long term solution to ensure a minimum safe heart rate is maintained.
- Symptomatic Bradycardia: A heart rate so slow it causes tiredness, dizziness, or fainting.
- Syncope: Sudden loss of consciousness followed by a rapid recovery.
- Pre-syncope: Feeling as though you are about to faint, often accompanied by blurred vision.
- Chronotropic Incompetence: When the heart cannot speed up to meet the body’s demands.
Clinical conditions requiring a pacemaker
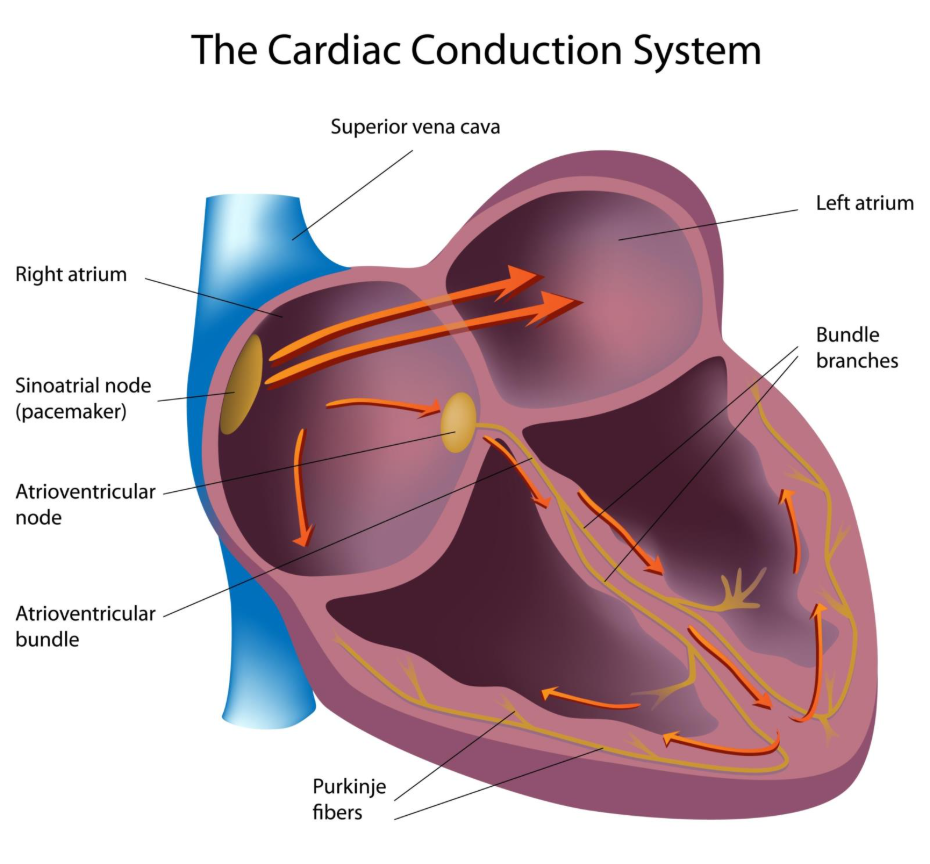
Fainting and slow heartbeats are frequently caused by two main conditions: heart block and sick sinus syndrome. Heart block occurs when the electrical signal is delayed or stopped as it moves from the top chambers (atria) to the bottom chambers (ventricles). Sick sinus syndrome occurs when the heart’s natural pacemaker, the sinoatrial node, does not fire signals consistently.
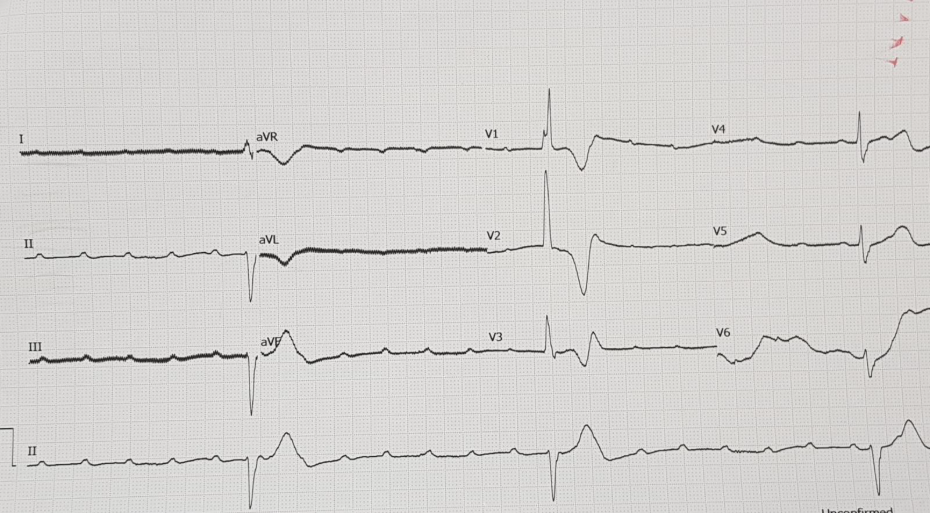
In the UK, NICE guidelines specify that high grade heart block (such as second or third degree block) is a primary indication for a pacemaker, especially if the patient is experiencing symptoms. These conditions are typically diagnosed using an electrocardiogram (ECG) or a wearable heart monitor (Holter monitor) that records the heart’s rhythm over 24 hours or longer to catch intermittent pauses that lead to fainting.
- First Degree Heart Block: A minor delay, rarely requiring a pacemaker.
- Third Degree (Complete) Heart Block: A total failure of signals, usually requiring an urgent pacemaker.
- Tachy-brady Syndrome: Alternating between very fast and very slow heart rates.
- Sinus Arrest: When the heart’s natural timer stops for several seconds at a time.
Causes of slow heart rate and fainting
The most frequent cause of these symptoms in the UK is age related degeneration of the heart’s conduction tissue. Over time, the electrical pathways can become scarred or ‘fibrotic,’ preventing signals from passing through. This is a common finding in individuals over the age of 65, though it can occur earlier in those with other heart conditions.
Other causes include damage from a previous heart attack, which leaves non conductive scar tissue in the heart muscle. Certain infections, such as Lyme disease or endocarditis, can also target the heart’s electrical system. Additionally, some medications used for high blood pressure or other heart issues, like beta blockers, can slow the heart rate to a level where a pacemaker becomes necessary to provide a safety net.
- Fibrosis: Natural scarring of the heart’s electrical system due to ageing.
- Ischaemia: Lack of blood flow or previous damage to the heart muscle.
- Medication Effects: Drugs that inadvertently slow the heart rate too much.
- Electrolyte Imbalance: Abnormal levels of potassium or calcium affecting electrical signals.
Triggers for fainting episodes
In patients with a borderline slow heart rate, certain triggers can cause the rate to drop further or lead to a fainting spell. Dehydration is a major trigger, as it reduces overall blood volume, making it harder for a slow heart to maintain blood pressure. Straining during a bowel movement or a sudden change in posture, such as standing up quickly, can also trigger a faint in susceptible individuals.
Extreme emotional stress or pain can occasionally trigger a ‘vasovagal’ response, which temporarily slows the heart and dilates blood vessels. While this is common and often benign, in someone with an underlying heart rhythm problem, it can be more severe and lead to more frequent episodes of syncope. Recognising these triggers is an important part of the diagnostic process.
- Dehydration: Low fluid levels causing a drop in blood pressure.
- Postural Changes: Moving from sitting to standing too rapidly.
- Physical Strain: Putting extra pressure on the heart and nervous system.
- Heat Exhaustion: High temperatures causing blood vessels to widen and pressure to drop.
Differentiating between heart-related and other faints
Not all fainting requires a pacemaker. It is important to differentiate between heart related (cardiac) syncope and other types, such as simple vasovagal faints or faints caused by low blood sugar. Cardiac faints often happen suddenly, without much warning, and can occur even while the person is sitting or lying down.
UK clinicians use a variety of tests to make this distinction. If a faint is accompanied by chest pain or happens during exercise, it is treated with higher urgency. A pacemaker is specifically designed to address faints caused by an electrical ‘slowdown’ or ‘blockage’ in the heart, and it is highly effective at preventing these episodes from recurring.
Conclusion
Fainting and a persistent slow heartbeat are significant symptoms that often indicate the heart’s electrical system needs support from a pacemaker. While a slow heart rate can be caused by many factors, including medication and ageing, a pacemaker provides a reliable way to prevent the brain from being deprived of oxygen. If you experience these symptoms, clinical investigation is essential to ensure your heart rhythm remains stable and safe.
If you experience severe, sudden, or worsening symptoms, such as a sudden blackout, crushing chest pain, or severe difficulty breathing, call 999 immediately.
Is a heart rate of 50 always an emergency?
Not necessarily; many healthy people have a resting heart rate in the 50s, but it becomes a concern if you feel dizzy, tired, or faint.
Can a pacemaker stop me from ever fainting again?
If your faints were caused by a slow heart rate, a pacemaker is very effective at preventing them, but it cannot prevent faints caused by other issues like low blood sugar.
What happens if I faint while the pacemaker is in?
Modern pacemakers record your heart rhythm; your clinical team can check the device to see if the faint was related to your heart or another cause.
Is the procedure to fit a pacemaker dangerous?
It is considered a very safe, routine procedure in the UK, usually performed under local anaesthetic in about an hour.
Will I have to stay in hospital long?
Most people go home the same day or the following morning after having a pacemaker fitted.
Can I still exercise with a slow heart rate?
You should wait for a clinical evaluation; if your heart cannot speed up during exercise, it may lead to fainting or severe shortness of breath.
Are there different types of pacemakers for this?
Yes, depending on where the ‘block’ is in your heart, you may need a single, dual, or triple chamber pacemaker.
Authority Snapshot
This article was written by Dr. Stefan Petrov, a UK trained physician with an MBBS and extensive experience in emergency medicine and intensive care. Dr. Petrov has managed acute cardiac cases and blackouts in hospital settings, performing the diagnostic tests necessary to identify the need for pacemakers. This content follows NHS and NICE safety guidelines to ensure accurate and balanced medical information for the public.

